|
Key Takeaways:
|
Cataracts are a significant cause of vision impairment worldwide, particularly in aging individuals. They develop when the proteins in the eye’s natural lens break down and clump together, leading to clouding of vision. Cataracts progress gradually and can interfere with daily activities, including reading, driving, and recognizing faces, and often lead people to consider cataract surgery when the condition starts affecting their routine.
Age is the main cause of cataracts but it’s not the only one. Some other risk factors for cataracts are age and family history that can’t be changed, while others sun/UV, smoking, diabetes or high blood sugar, long-term steroid use, eye injuries, heavy alcohol use, and poor diet can be managed.
This guide explains what causes cataracts, who is at higher risk, and the prevention steps that make a real difference.
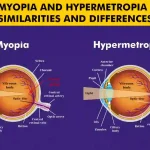
What Is a Cataract?
A cataract is an eye condition when the eye’s clear lens becomes cloudy. This makes vision blurry, causes glare from lights, and can make night driving hard.
The clouding happens as lens proteins change over time. Cataracts usually grow slowly. If they become severe and are not treated, they can lead to major vision loss.
The good news is that cataracts are common and treatable, your eye doctor can guide timing and options.
Common Risk Factors for Cataracts
Cataracts can develop for many reasons; knowing what causes them, how each cause affects the lens, and the key facts helps you act early and protect your vision.
|
Factor |
How does it drive cataracts? |
Who’s at higher risk? |
Evidence strength* |
|
Ageing |
Lifelong oxidative stress makes lens proteins cross-link; the clear lens gradually turns opaque. |
60+ years; earlier in physically demanding outdoor jobs. |
High |
|
Genetics / family history |
Inherited lens protein variants or weaker repair systems speed clouding. |
First-degree relatives of people with nuclear cataract; certain ethnic clusters. |
High |
|
UV exposure (sunlight) |
UV-A/UV-B trigger free-radical damage and protein aggregation in the lens. |
Outdoor workers, high-altitude or tropical regions. |
High |
|
Smoking |
Toxins deplete antioxidants (e.g., glutathione) and raise free radicals in the lens. |
Current/ever smokers; pack-years correlate with risk. |
High |
|
Heavy alcohol use |
Lowers systemic antioxidants; metabolic by-products stress lens fibers. |
Binge/heavy users; coexisting poor diet. |
Moderate |
|
Diabetes / poor glycaemic control |
High glucose glycosylates lens proteins and draws water into the lens (osmotic swelling). |
Long-standing diabetes, high HbA1c, early-onset diabetes. |
High |
|
Hypertension / metabolic syndrome / obesity |
Vascular & oxidative stress accelerate lens opacity formation. |
People with MetS (central obesity + BP + lipids). |
Moderate–High |
|
Eye injuries (trauma) |
Capsule/fiber disruption → rapid “traumatic” cataract. |
Sports, industrial work without eye protection. |
High |
|
Long-term corticosteroids (systemic, inhaled, topical, intraocular) |
Alters lens epithelial metabolism → typical posterior subcapsular cataract (PSC). |
Long duration/high dose; combined routes (e.g., inhaled + oral). |
High |
|
Other medications(selected) |
Some drugs alter lens metabolism/oxidative balance. |
Long-term miotics, phenothiazines; rare idiosyncratic cases. |
Low–Moderate |
|
Previous eye surgery(e.g., vitrectomy) |
Changes ocular oxygen dynamics, speeding nuclear sclerosis. |
Post-vitrectomy eyes; gas/oil tamponade exposure. |
Moderate–High |
|
Chronic uveitis / ocular inflammation |
Inflammatory cytokines and steroid treatment both raise cataract risk. |
Recurrent uveitis; autoimmune conditions. |
High |
|
Radiation exposure(ionising/infrared heat) |
Direct damage to lens epithelium; “glassblower’s” cataract with IR. |
Radiotherapy to head/neck; foundry/glass workers. |
High |
|
Indoor smoke / biomass fuels |
Persistent oxidant load from cooking fuels and kerosene lamps. |
Households using biomass; poorly ventilated kitchens (common in parts of India). |
Moderate–High |
|
Poor diet (low antioxidants/carotenoids) |
Less defence against oxidation; faster lens protein damage. |
Diets low in vitamin C, lutein, zeaxanthin. |
Moderate |
|
High myopia |
Elongated eye alters lens environment; earlier nuclear changes. |
Axial myopia >-6.00D. |
Moderate |
|
Atopic dermatitis / eczema |
Chronic inflammation & steroid use predispose to anterior/posterior changes. |
Severe, long-standing atopy. |
Moderate |
|
Socio-economic factors |
Late presentation, outdoor work, limited access to UV protection and care. |
Rural/low-resource settings. |
Moderate |
Age and Cataract Formation
Age is the biggest answer to what causes cataracts. As we grow older, the clear lens in the eye changes: its proteins clump, the lens hardens and turn yellow, and light scatters. This slow change is why many people notice glare at night or hazy vision first. Age-related cataracts affect both eyes, though not always at the same time.
By late life this is very common: more than half of people aged 80+ have a cataract or have had cataract surgery, which is why age is the top cataract risk factor. While aging can’t be stopped, you can still lower cataract risk factors you can control. Good sun protection, no smoking, and regular eye checks help you spot changes early. If daily tasks become hard, your eye doctor will discuss safe treatment options.
Genetic Predisposition
Family history is one of the risk factors for cataracts you can’t change. Some people inherit lens traits that make the lens less stable with time. In a few cases, babies are born with congenital cataracts, or children develop them early due to genetic conditions or infections in pregnancy.
If a sibling has nuclear cataract, your own odds are about 2× higher; some cataracts also start in childhood, with congenital cataract occurring in roughly 1–3 per 10,000 births worldwide.
If close relatives had cataracts at a younger age, tell your eye doctor. You may need earlier or more frequent eye exams. Knowing your family history helps you act sooner on the causes of cataract you can control.
Prolonged UV Exposure
Too much sunlight, especially UV adds oxidative stress to the lens and speeds clouding. This is a common, preventable part of why cataract happens.
The risk is higher if you work outdoors, live at high altitude, or spend long hours near reflective surfaces like water or snow. Global health data suggest up to ~10% of cataracts may be due to excess UV. Protecting your eyes is simple. Wear UV400 sunglasses (look for 100% UVA/UVB on the label) and a wide-brim hat.
Even on cloudy days, UV can reach your eyes, so make eye protection a habit.
Smoking and Alcohol Consumption
Smoking raises oxidative stress inside the eye and is a well-known cataract risk factor. Over time, it damages lens proteins and speeds clouding, which is why smokers get cataracts earlier and more often.
Meta-analyses show smoking is linked to nuclear cataract (OR ~1.7–1.9) and that heavy current smokers had about a 42% higher risk of cataract extraction versus never-smokers;
The good news: risk starts to drop after quitting. For alcohol, heavy use can lower the body’s natural antioxidants and may increase cataract risk, while moderate intake shows no clear overall increase. If you drink, keep it moderate and focus on overall eye-healthy habits. Cutting tobacco and limiting alcohol work together to reduce risk factors for cataracts.
Diabetes and Other Health Conditions
High blood sugar changes the lens environment and draws water into the lens, making it swell and cloud. People with diabetes often develop cataracts earlier. Other conditions, like high blood pressure, obesity, and metabolic syndrome, also add stress to the lens.
A meta-analysis found type 2 diabetes nearly doubles the odds of cataract (OR ~1.97). Hypertension and metabolic syndrome also add risk (e.g., MetS RR ~1.28), so controlling general health helps prevention.
Keeping HbA1c in target, taking medicines on time, and getting regular eye exams reduce these cataract risk factors. Managing general health is a strong part of prevention for your eyes and the rest of your body.
Eye Injuries and Trauma
Blunt hits, penetrating wounds, or chemical splashes can disrupt the lens or its capsule and lead to a traumatic cataract. Sometimes clouding shows up right away; other times it appears months later. Sports like cricket or racquet games, certain factory jobs, and DIY tasks carry higher risk.
Eye injuries are common (lifetime ocular-trauma prevalence ~14%), and up to ~65% of eye traumas can lead to cataract. Simple protection goes a long way. Wear proper safety glasses or a face shield when needed. If an injury happens, get urgent eye care, even if vision seems okay, so delayed problems don’t develop.
Prolonged Use of Corticosteroids
Long-term or high-dose steroids (tablets, some inhalers, skin creams around the eyes, or frequent steroid eye drops) can cause a type called posterior subcapsular cataract. This can blur near vision and cause glare faster than age-related changes.
Risk rises with dose and duration: one analysis reported PSC odds about 2.5× with inhaled steroids and 4.1× with oral steroids (adults, Australia).
Always adjust the dose only with your doctor. Never stop a prescribed steroid suddenly. Instead, speak with your doctor about the lowest effective dose and regular eye monitoring.
Dietary and Nutritional Deficiencies
A diet low in antioxidants leaves the lens with less protection from everyday wear and tear. Nutrients like vitamin C, vitamin E, lutein, and zeaxanthin support lens health, while omega-3s help overall eye comfort.
A twin study reported diets rich in vitamin C were linked to a ~33% lower risk of cataract progression. Food usually beats pills. Aim for leafy greens (spinach, kale), colourful vegetables and fruits, nuts and seeds, and fatty fish like salmon.
Over time, these choices support the lens and fit into simple prevention for cataracts.
Complications of Cataract Surgery with Glaucoma
When glaucoma and cataract are both present, surgery planning needs extra care. Eye pressure (IOP) can change during and after surgery, and a fragile optic nerve may be more sensitive to spikes.
Early IOP spikes are a known issue; reports show many peaks occur 8–12 hours after surgery, and 1.3–10% of cases still measure >30 mmHg at 24 h (population and technique dependent). Some patients may need pressure-lowering drops adjusted or combined procedures if advised.
Close follow-up matters. Your surgeon will choose techniques and lens options that protect the optic nerve, set a safe target IOP, and schedule more checks early in recovery. With careful planning, most people do well, even with these added risk factors.
Cataract Risk Factors & Everyday Prevention
Understanding cataract risk factors makes the picture clear. Some parts of what causes cataracts like age and family history cannot be changed, but many can be managed.
Sunlight, smoking, high blood sugar, long-term steroid use, injuries, poor diet, and indoor smoke all add stress to the lens and raise risk.
Simple prevention helps like protecting your eyes from UV, not smoking, keeping diabetes and blood pressure controlled, eating leafy greens, fruits, nuts, seeds, and fish, using safety eyewear at work or sport, and reviewing long-term medicines with your doctor.
Regular eye checks then keep track of changes and timing for care. With steady habits, you can lower risk factors for cataracts and keep clearer, more comfortable vision for longer.
FAQs
What are the disadvantages of cataract surgery?
The disadvantages of cataract surgery are a small risk of infection or swelling, possible glare/halos at night, and a chance of a thin film forming behind the new lens (PCO) that may need a quick laser fix later.
Is cataract surgery painful?
No, cataract surgery is not painful because numbing drops or local anesthesia are used; you may feel gentle pressure, not pain. Afterward, the eye can feel scratchy or sore for a day or two and improves with the prescribed drops.
What is the most common complication of cataract surgery?
The most common complication of cataract surgery is posterior capsule opacification (PCO), a thin, cloudy film that can blur vision months or years later. It’s fixed in minutes with a simple outpatient YAG laser treatment.
Is eye cataract dangerous?
Yes, cataract is dangerous as it blurs vision and can affect driving, reading, and safety. If left very long, it can rarely raise eye pressure or cause inflammation.
Does cataract surgery have side effects?
Yes, cataract surgery does have side effects, most short-term: redness, light sensitivity, dry eye, or mild floaters. Serious issues are uncommon, and most people heal over a few weeks with proper do’s & don’ts after cataract surgery and follow-up care.