Table of Contents
- Understanding Glaucoma: A Silent Vision Thief
- The Science Behind Neuroprotection
- Traditional vs. Neuroprotective Approaches in Glaucoma
- Emerging Therapies: What’s on the Horizon?
- Clinical Trials and Research: Progress and Challenges
- The Role of Lifestyle and Systemic Health
- Practical Steps for Patients: Managing Glaucoma Today
- Potential and Limitations of Neuroprotection
- Looking Ahead: The Future of Neuroprotection in Glaucoma
- Conclusion
- FAQs
Glaucoma is often called the “silent thief of sight” for a reason; it usually causes no pain, few symptoms, and steals vision slowly, often before the patient even knows it. Globally, it is one of the most common causes of irreversible blindness. For many years, lowering intraocular pressure (IOP) has been the focus of glaucoma surgery. However, even with perfectly managed pressure, some patients still lose sight. This has inspired a growing clinical movement toward a new frontier: neuroprotection. This blog will help you understand the science behind glaucoma neuroprotection therapy, explore emerging therapies, highlight the importance of lifestyle factors, and give you practical advice for preserving your vision.
Understanding Glaucoma: A Silent Vision Thief
Glaucoma is a group of eye disorders that causes optic nerve damage, the vital “nerve” that transmits visual information from the eye to the brain. The main cause of damage is usually high IOP, but factors like blood flow, genetics, and cellular health all play a role. Most types of glaucoma progress silently until late stages; so, early, regular eye check-ups are critical.
The optic nerve is made up of more than a million nerve fibers. In glaucoma, retinal ganglion cells (RGCs) are lost over time, resulting in progressive peripheral vision loss and, eventually, central blindness if untreated. Unfortunately, once optic nerve fibers are destroyed, they don’t regrow, making any lost vision permanent.
The Science Behind Neuroprotection
Neuroprotection refers to strategies that aim to preserve nerve cell health, slow degeneration, and protect remaining function, even beyond controlling eye pressure. For glaucoma, this means saving the retinal ganglion cells and further optic nerve damage, regardless of IOP.
New research reveals that optic nerve cells are vulnerable not only to pressure but also to poor blood supply, inflammation, oxidative stress, and energy production failures. Neuroprotective therapy aims to block these threats and keep nerve cells functioning. Scientists investigate medications, genetic therapies, and even cell-based approaches to defend RGCs and restrict optic nerve damage.
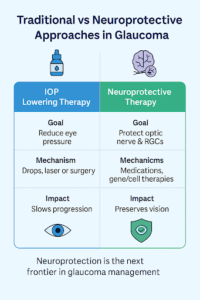
Traditional vs. Neuroprotective Approaches in Glaucoma
Emerging Therapies: What’s on the Horizon?
The neuroprotective field is growing rapidly, and several therapy classes are being explored in clinical studies and early trials:
Pharmacological Treatments
- Neurotrophic Factors: These promote the survival and regeneration of nerve cells. Brain-derived neurotrophic factor (BDNF) and ciliary neurotrophic factor (CNTF) are currently under investigation.
- Antioxidants: Vitamins (like C and E), as well as new compounds, aim to fight oxidative stress, a key player in optic nerve damage.
- NMDA Receptor Antagonists: These drugs block a brain signaling pathway thought to be toxic in glaucoma, e.g., memantine.
- Calcium Channel Blockers and Alpha-2 agonists: These may enhance blood flow and further support nerve health in selected patients.
Gene Therapy
Several experimental treatments aim to “switch on” protective genes within retinal cells or supply new genes that help nerve survival. Techniques are mostly in early study or animal trials, but hold promise for hard-to-treat glaucoma types.
Regenerative Medicine
Stem cell transplantation to replace lost RGCs or deliver neurotrophic support is an exciting avenue under active study, though not yet available in routine practice.
Clinical Trials and Research: Progress and Challenges
Clinical trials are vital for learning what works, and what may not, in neuroprotection. Trials in the US, Europe, and Asia are investigating neurotrophic agents, new drug classes, stem cell treatments, and advanced drug delivery systems, such as slow-release implants or crosses of blood-brain/retina barriers.
Some drugs, like memantine, have shown mixed results in recent studies, highlighting that not every approach is a breakthrough. But continued research, especially with combination therapies and personalized treatment, is expected to shape better outcomes in the coming years.
The Role of Lifestyle and Systemic Health
While neuroprotection often focuses on medication or genetic therapy, patients shouldn’t overlook basic health care:
- Blood Pressure: Both high and low blood pressure can affect optic nerve health; maintaining stable, healthy BP is best.
- Exercise: Regular aerobic activity may improve eye blood flow and overall nerve health.
- Managing Diabetes and Cholesterol: Poorly controlled diabetes or high cholesterol can damage blood vessels supplying the eye.
- Diet: Diets rich in leafy greens, fruits, and antioxidant-rich foods support retinal and nerve health.
Practical Steps for Patients: Managing Glaucoma Today
Regardless of the exciting field of neuroprotection, everyday care is still critical:
- Stick to prescribed eye drops: Pressure control is proven to protect vision.
- Attend all follow-up appointments: Early signs of new damage can only be caught in the clinic.
- Discuss any side effects: Some medications for IOP or neuroprotection may cause local or systemic side effects; don’t adjust or stop without your doctor’s advice.
- Share all your health information: Strong family history, other medical conditions, or struggles with side effects all matter in fine-tuning your plan.
Potential and Limitations of Neuroprotection
It’s vital to recognize that neuroprotection is meant to slow or reduce damage, not to reverse vision loss. While it may preserve more of your vision, it is unlikely to restore what is already gone. Treatments remain in early stages for most drugs, and much more research is needed to bring these options to everyday clinics.
Still, clinical evidence is growing, and combined strategies are emerging as standard of care for patients not achieving goals with pressure control alone.
Looking Ahead: The Future of Neuroprotection in Glaucoma
The future looks clear and bright for glaucoma patients as more interdisciplinary research unites genetics, pharmacology, and bioengineering. Neuroprotective strategies will likely become part of a “multi-pronged” approach, including IOP lowering, neurotrophic support, gene-based management, and systemic health optimization.
Greater emphasis on patient monitoring, earlier detection, and individualized risk assessment is expected. In the next decade, eye care specialists hope to offer neuroprotective therapies alongside standard pressure reduction for every patient at risk of vision loss from glaucoma.
Conclusion
While pressure reduction remains the mainstay, the potential for neuroprotection offers real hope to reduce vision loss, especially for high-risk and advanced cases. Staying informed, actively managing overall health, and working closely with your eye care team can maximize your chances of a safe, independent, and visually rich future. Ongoing research brings new promise, ensuring that in the fight against glaucoma, the future is focused on both saving and protecting sight.