|
Key Takeaways:
|
Cataract grading is how doctors measure how cloudy the lens is, where the haze sits (centre, edges, or back), and how much it affects vision, usually using a simple scale (like 1–4/1–5 or LOCS III), so everyone describes the cataract the same way.
The numbers and names can be confusing; terms like cataract classification, nuclear/cortical/PSC, and the stages of cataract may not make sense at first.
This guide explains the cataract grading scale (1–5), outlines what each grade means for vision, and provides a quick chart to help you understand what to expect.
What is Cataract Grading?
Cataract grading is a scale on which an eye doctor measures how cloudy your lens is, where the clouding sits (center, edges, or back of the lens), and how much it affects vision. Doctors examine the lens at the slit lamp after dilating the pupil and record the type (nuclear, cortical, or posterior subcapsular (PSC)), as well as the severity, using a standard chart or scale.
This helps determine when to treat and which options are the best fit for the patient. Grading looks at 3 (three) factors:
- Location of the haze (nucleus/center, cortex/outer rim, or back under the capsule)
- Amount of haze (mild to advanced)
- Impact on vision (glare, night driving, reading, test results).
Most clinics use a recognized cataract grading system, along with photo standards (LOCS III), so that different doctors can describe the cataract the same way.
History of Cataract Grading
Below is the history of the cataract grading system:
- Before standardized systems: Cataracts were described in broad terms (present/absent, mild/severe), which made comparison between patients and clinics hard.
- LOCS era: Researchers built the Lens Opacities Classification System; the most used version today is LOCS III (1993).
It uses standard photographs to grade: nuclear colour (NC) and nuclear opalescence (NO) from slit-lamp images, and cortical (C) and PSC (P) from retro-illumination images, improving agreement between doctors.
- WHO simplified system: For field and program settings, the WHO/Thylefors group published a simplified cataract grading system so graders with basic training could record cataract types and severity reliably.
- Modern tools: Clinics and studies now add objective imaging.
For example, Scheimpflug (Pentacam) lens densitometry or the double-pass scatter index to quantify lens haze and track change, alongside clinical grading.
|
Why is Cataract Grading Important? A clear, shared classification (LOCS III or WHO simple scales) plus modern imaging makes grading repeatable across visits and doctors, which improves the decisions of doctors about the timing of surgery. |
How is Cataract Grading Performed?
Doctors grade cataracts during a comprehensive eye exam.
- First, they check visual acuity (how small you can read on a chart) and refraction.
- Then, they test glare/brightness sensitivity (e.g., with a Brightness Acuity Tester) because cataracts can cause a greater decline in vision in bright light.
- After dilating the pupil, they examine the lens using the slit-lamp microscope and record where the haze sits, nuclear, cortical, or posterior subcapsular (PSC), and how dense it is using a standard grading chart.
- Many clinics also capture photos (including retro-illumination for cortical/PSC) and may add objective imaging to quantify lens density.
Scheimpflug (Pentacam) densitometry and similar tools correlate well with standard clinical grades (LOCS III), and newer devices (e.g., IOLMaster 700 lens density) are being studied for objective severity scales. These measurements help track change and plan timing for cataract surgery.
Types of Cataract Grading Systems
Below are the different types of cataract grading systems:
- LOCS III (Lens Opacities Classification System III): The most widely used clinical/research standard.
It utilises reference photographs to grade nuclear colour (NC) and nuclear opalescence (NO) at the slit lamp, as well as cortical (C) and PSC (P) from retro-illumination images, thereby improving agreement between doctors.
- Oxford Clinical Cataract Classification and Grading System: An earlier, slit-lamp–based system using standard diagrams and colour samples to grade multiple cataract features in equal intervals.
It helped set the stage for modern photographic systems.
- WHO Simplified Cataract Grading System: A field-friendly system designed for programmes and surveys so trained staff can grade common cataract types reliably with basic equipment.
|
Bottom line LOCS III is the go-to in clinics and studies; Oxford is valuable historically; WHO is useful for public health screening and reporting. |
Components of Cataract Grading (What Doctors Record)
Below are the different components of the cataract grading system:
- Location/pattern: Nuclear (centre), cortical (spokes from the rim), or PSC (at the back under the capsule). This helps explain symptoms like night glare or near-vision trouble.
- Density/opacity: Graded from mild to advanced using photo standards (e.g., LOCS III) so different doctors can describe the same cataract the same way.
- Impact on vision: Visual acuity, glare testing, and contrast sensitivity may be noted, as some cataracts (e.g., PSC) reduce vision more significantly in bright light.
Cataract Grading Chart
Doctors use a patient-friendly scale of 1–4 to explain severity (some clinics use 1–5 or the LOCS III photo scale so that numbers may differ by clinic).
|
Grade |
What the doctor sees |
What you notice |
|
1 (Mild) |
Early, patchy clouding |
Slight blur, extra glare, fine at most tasks |
|
2 (Moderate) |
Clearer lens changes in the center/rim/back |
Noticeable blur, night glare, harder small print |
|
3 (Severe) |
Dense clouding; detail at the back of eye harder to see |
Reading/driving difficult; colours dull; safety concerns |
|
4 (Very severe) |
Lens mostly/fully opaque (mature); may look white |
Vision very poor or only light perception |
Remember: Grading is only one part of the decision. Your symptoms, daily needs (work/driving), other eye diseases, and test results all guide when to treat.
Challenges and Limitations of Cataract Grading
Below are the different challenges and limitations of the cataract grading system:
- Grading can be subjective. Two examiners might score the same lens slightly differently, even with photo standards. Lighting, pupil size, and camera settings also affect how the lens looks.
- Numbers don’t tell the whole story. Some people with a “mild” grade struggle a lot (e.g., strong glare with a small PSC), while others function well despite a higher grade. Your job, night driving, and reading matter.
- Other eye issues change the picture. Macular degeneration, glaucoma, corneal problems, or long-standing diabetes can reduce vision independent of the cataract grade.
- Different scales exist. Your clinic may use 1–4, 1–5, or LOCS III photo grades for nuclear/cortical/PSC. The labels differ, but the goal is the same: to describe severity clearly and choose the right time for surgery.
Conclusion
Cataract grading converts what the doctor sees into clear numbers and names, making timing and treatment easier to plan. Your clinic may use a 1–4 or 1–5 scale, but the idea is the same: record where the clouding sits (nuclear, cortical, PSC), how dense it is, and how much it affects daily life (reading, screens, night driving). Use the grade as a guide, not a rule, along with your symptoms, job needs, and other eye conditions to determine when to treat.
FAQs
What are the grades of cataracts?
The grades of cataracts are simple severity steps, usually ranging from 1 (mild) to 4 (very severe), or 1–5 in some clinics, showing how cloudy the lens has become and how much it affects vision.
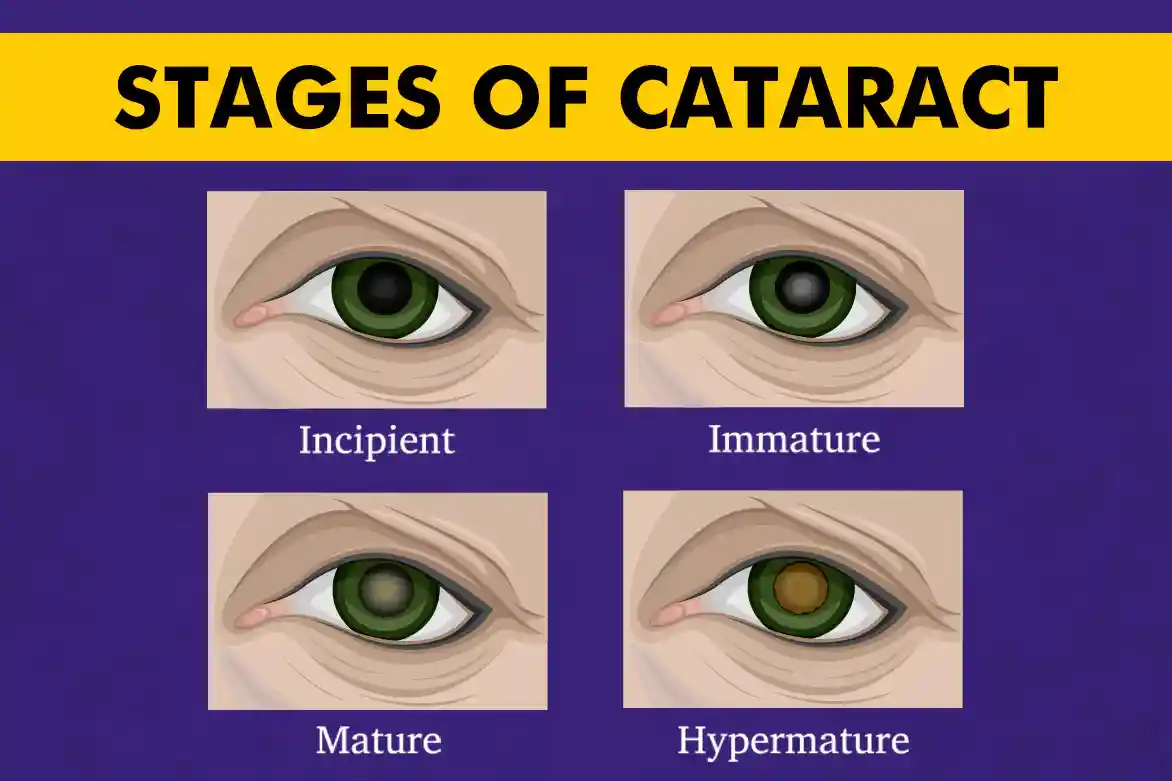
What are the 4 stages of cataract?
The 4 stages of cataract are early/incipient (immature), progressing (still immature), mature, and hypermature, progressing from small cloudy areas to a lens that is mostly or fully opaque.
What is a Grade 4 cataract?
A Grade 4 cataract is a very severe cataract with the lens mostly/fully cloudy; vision is very poor, and surgery is usually advised soon.
What is stage 3 cataract?
Stage 3 cataract is a severe cataract characterised by dense clouding that makes reading, driving, and performing daily tasks difficult; doctors typically recommend surgery.
What is cataract grading?
Cataract grading is the systematic scoring of lens clouding, by location (nuclear, cortical, PSC) and density, to show severity and guide treatment timing.
What is the classification of cataracts?
The classification of cataracts includes:
- Pattern-based types: nuclear, cortical, posterior subcapsular (PSC)
- Cause-based types: age-related, congenital/pediatric, traumatic, secondary (e.g., diabetes, steroids), and radiation.
What factors are considered in cataract grading?
The factors considered in cataract grading are where the haze sits in the lens, how dense it is, and how it affects vision (visual acuity, glare/contrast, night driving).
How does cataract grading influence treatment decisions?
Cataract grading influences treatment decisions by pairing the grade with your symptoms and needs; higher grades and a greater day-to-day impact tend to push toward earlier surgery, while lower grades with minimal symptoms may be monitored.
How does cataract grading differ from cataract diagnosis?
Cataract grading differs from cataract diagnosis because diagnosis states “you have a cataract,” while grading indicates “how severe it is, where it is, and how much it affects vision,” which helps determine when to treat.