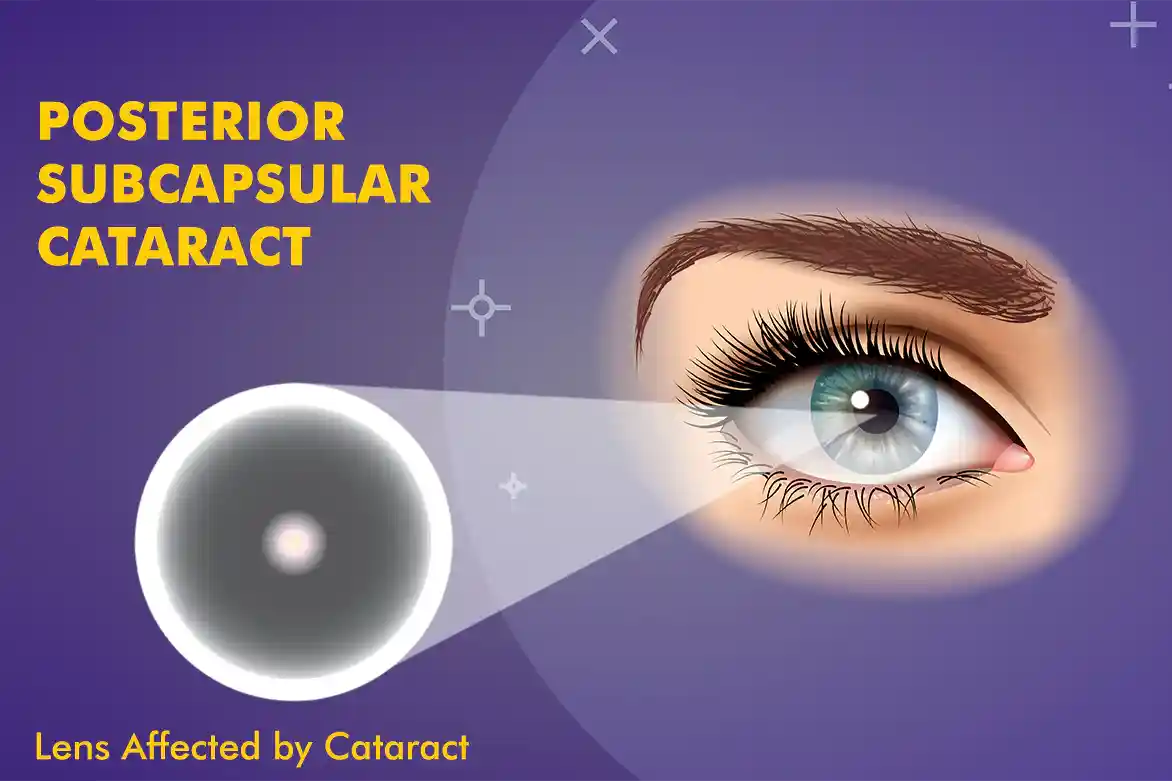
Meaning of Posterior Subcapsular Cataract (PSC)
A posterior subcapsular cataract (PSC) is a type of cataract that forms at the back of the eye’s natural lens, just in front of the posterior capsule that encases the lens.
Unlike other cataract types, which may affect the centre (nuclear) or edges (cortical) of the lens, PSC specifically targets the back layer. This location is critical because it lies directly in the path of light entering the eye, which can significantly interfere with vision, particularly in bright environments or while reading.
In medical practice, PSC is often more visually disabling than other types of cataracts, even when smaller in size. Individuals frequently report a sudden onset of symptoms rather than a slow progression, making it an important diagnosis in clinical ophthalmology.
Anatomy of the Lens
While it may sound complicated, to understand the implications of a posterior subcapsular cataract, it is essential to grasp the basic structure of the crystalline lens. Let’s break it down below.
The lens is a transparent, flexible structure positioned just behind the iris. It helps focus light onto the retina, enabling sharp vision. It is enclosed by a thin capsule, which protects the inner lens fibres. The front part is known as the anterior capsule, and the back is the posterior capsule.
PSC occurs in the subcapsular space just beneath the posterior capsule. This region is densely populated by epithelial cells that can undergo abnormal changes, leading to opacification. These opacities disrupt the passage of light and may lead to significant visual impairment.
How PSC Develops
Posterior subcapsular cataracts typically develop when abnormal migration and proliferation of epithelial cells occur at the back of the lens. These cells cluster together and form granular or plaque-like opacities. The cause of this abnormal cellular behaviour can vary depending on underlying factors, which may include systemic health conditions, medications, trauma, or radiation exposure.
Unlike nuclear cataracts, which evolve over several years, PSC tends to progress more rapidly. It may also present bilaterally, affecting both eyes, especially when linked to systemic causes or long-term steroid use.
Common Causes of PSC
A variety of factors may contribute to the formation of PSC. Some are iatrogenic (treatment-induced), while others stem from internal physiological processes.
Understanding the underlying posterior subcapsular cataract can help in identifying at-risk individuals and tailoring prevention strategies. The most frequently encountered causes include:
Prolonged Corticosteroid Use
Long-term systemic or topical steroid therapy is one of the leading causes. Both oral corticosteroids (e.g., prednisone) and inhaled variants used in chronic asthma can contribute to PSC development.
Diabetes Mellitus
Patients with poorly controlled diabetes are at a higher risk. Elevated blood sugar can alter lens metabolism and promote posterior lens changes.
Ocular Trauma
Blunt trauma to the eye can accelerate lens fibre damage and prompt posterior cataract formation. PSC is one of the more common cataract types seen post-injury.
Radiation Exposure
Patients undergoing radiation therapy to the head or neck, or those exposed to ultraviolet radiation over time, may experience cellular changes in the lens leading to PSC.
Risk Factors Associated with PSC
While causes are linked to specific mechanisms, risk factors refer to predisposing conditions or demographics. The following are well-documented risk contributors:
- Age (commonly after 40, but can appear earlier in certain cases)
- Chronic steroid use (inhaled, oral, or topical)
- Systemic conditions (such as lupus or sarcoidosis)
- Family history of cataracts
- Previous eye surgery or inflammation (e.g., uveitis)
- Exposure to ionising radiation or UV light
Regular ophthalmic monitoring is recommended for patients presenting with multiple risk factors.
Symptoms
The visual effects of a posterior subcapsular cataract are often more pronounced than other types, despite the cataract’s relatively small size. Commonly reported posterior subcapsular cataract symptoms include:
- Blurry or hazy vision, especially in bright light
- Difficulty reading, particularly small print
- Glare or halos around lights at night
- Reduced contrast sensitivity
- Rapid visual decline, often more noticeable in one eye
- Increased sensitivity to sunlight or bright indoor lighting
These symptoms tend to intensify during activities requiring focused vision, such as reading, computer use, or driving at night.
Diagnosis
Diagnosing a posterior subcapsular cataract involves a comprehensive eye examination. The process includes:
Visual Acuity Testing
A standard Snellen chart is used to assess the degree of vision impairment.
Slit Lamp Examination
A slit lamp provides a magnified view of the anterior and posterior lens structures. PSC typically appears as a grainy or plaque-like opacity at the back of the lens.
Dilated Fundus Examination
Although PSC affects the lens and not the retina, dilation helps assess whether there are any additional ocular pathologies coexisting with the cataract.
In early stages, observation may suffice. In advanced cases, referral for posterior subcapsular cataract treatment is typically indicated.
Progression and Impact
The natural history of PSC varies. In some cases, the cataract remains stable for months or even years, while in others, it progresses swiftly. Because of its position at the visual axis, even minor changes can have a disproportionate impact on quality of life.
Activities such as night driving, reading, or working under fluorescent lighting often become increasingly difficult. Patients may experience a decline in their ability to perform daily tasks, prompting consideration of posterior subcapsular cataract surgery.
Treatment Options
The first step is to always schedule an appointment with an eye specialist to understand the optimum strategy for treatment. Management depends on the severity of symptoms and the degree of visual disruption. Conservative options may offer temporary relief, but definitive care typically involves surgery.
Non-Surgical Approaches
- Stronger prescription lenses may help during the early stages
- Anti-glare glasses can minimise light sensitivity
- Lifestyle adjustments such as limiting night driving or increasing font sizes on digital devices
However, these measures do not halt the progression of PSC. For patients who continue to experience visual limitations, surgical treatment becomes necessary.
Surgical Approach
When non-invasive treatments are no longer effective, cataract extraction becomes the gold standard. Posterior subcapsular cataract surgery involves:
Phacoemulsification
This is the most commonly used technique. It involves breaking the cataract into tiny fragments using ultrasonic waves, followed by removal through a small incision. A synthetic intraocular lens (IOL) is then implanted in the capsular bag. Advanced technologies like the femtosecond laser-assisted cataract surgery are now available for the treatment of posterior subcapsuslar cataract.
Intraocular Lens Selection
Patients may choose from monofocal, multifocal, or toric lenses based on their vision goals and eye health.
Outpatient Procedure
PSC surgery is typically done on an outpatient basis, requiring only local anaesthesia. Recovery times are usually short, and many patients report substantial improvement in vision within a few days.
Recovery and Aftercare
Postoperative care is crucial to ensure successful outcomes. After posterior subcapsular cataract surgery, the following steps are essential:
- Use of prescribed eye drops (usually antibiotics and corticosteroids)
- Avoiding heavy lifting or bending during the initial recovery period
- Wearing protective eyewear to prevent accidental injury
- Following up with scheduled eye exams to monitor healing and vision improvement
Patients are generally able to return to routine activities within a week, although full visual stabilisation may take a few weeks.
Living With PSC
Not all patients with PSC require immediate surgery. Some adapt well with minor lifestyle adjustments. For those with early-stage PSC:
- Use brighter lighting when reading
- Adjust computer screens to reduce glare
- Wear hats and UV-protective sunglasses when outdoors
- Keep systemic conditions, like diabetes, under control
Being proactive can help preserve vision and delay the need for surgical intervention.
Prevention Tips
While not all cases are preventable, certain steps can reduce risk or slow progression:
- Limit corticosteroid use to essential cases and the shortest duration
- Manage chronic illnesses (e.g., diabetes, autoimmune disorders)
- Protect eyes from excessive sunlight with UV-blocking lenses
- Undergo regular eye exams, especially if in a high-risk group
- Avoid smoking, which is linked to earlier cataract formation
A proactive lifestyle, including eye-friendly nutrition and protective habits, plays a crucial role.
Read on to understand more about how to prevent cataracts and tips to lead a healthy life.
Posterior subcapsular cataract may present with subtle symptoms but can greatly interfere with vision due to its strategic location on the lens. Recognising the early signs, understanding the posterior subcapsular cataract causes, and knowing when to consider treatment can make a meaningful difference in preserving vision and quality of life.
If you’re experiencing glare, difficulty reading, or struggling with night vision, it might be time to consult an eye care professional for a thorough evaluation.
Preserve your vision with clarity and confidence. Schedule A Cataract Evaluation
FAQs
What is the main causes for posterior subcapsular cataract?
Aging, prolonged steroid use, diabetes, and eye trauma are common causes of Posterior Subcapsular Cataract.
What are the common symptoms to watch for Posterior Subcapsular Cataract?
Watch for blurred vision, increased glare sensitivity, difficulty with night vision, halos around lights, and reduced contrast sensitivity.
How is Posterior Subcapsular Cataract diagnosed?
Posterior Subcapsular Cataract is diagnosed through a comprehensive eye examination, including visual acuity tests and a dilated eye exam.
What treatment options are available for Posterior Subcapsular Cataract?
Posterior subcapsular cataract surgery, involving the removal of the cloudy lens and implantation of an intraocular lens, is the primary posterior treatment for Posterior Subcapsular Cataract.
What is the recovery process like after cataract surgery for posterior polar cataracts?
After cataract surgery, patients typically experience improved vision shortly and achieve complete recovery within a few weeks.
Are there any complications associated with cataract surgery for posterior polar cataracts?
While uncommon, risk of cataract surgery may include infection, bleeding, or changes in eye pressure.
Can posterior polar cataracts recur after cataract surgery?
Posterior polar cataracts generally do not recur after successful cataract surgery.
Can a posterior subcapsular cataract be fixed?
Yes, posterior subcapsular cataracts can be treated with surgery for visual improvement.
How fast do posterior subcapsular cataracts grow?
The growth rate of posterior subcapsular cataracts varies, but they tend to progress faster than other types.
Where is the posterior subcapsular area?
The posterior subcapsular area is the back part of the lens capsule, where these cataracts typically form.
What causes a posterior subcapsular cataract to form compared to other cataract types?
Unlike other cataract types, PSC can form due to factors like long-term steroid use, diabetes, radiation exposure, and eye trauma. The condition arises when abnormal cells accumulate at the back of the lens. If you’d like to know more about variations in cataract, check out our detailed guide on cataract surgery types.
What are the early signs of posterior subcapsular cataract?
Early signs include glare in bright lights, blurry vision while reading, difficulty with contrast, and seeing halos around lights, particularly at night.
Is surgery always required for posterior subcapsular cataracts?
Not always. Mild cases can be managed with glasses and environmental adjustments. Surgery is considered when vision significantly affects daily activities.
How successful is posterior subcapsular cataract surgery?
Outcomes are generally favourable, but vary based on individual eye health, choice of intraocular lens, and adherence to post-operative care.
Can posterior subcapsular cataracts come back after surgery?
No, the cataract itself cannot return. However, some patients may develop a secondary condition called posterior capsule opacification, which can be treated with a quick laser procedure.