Table of Contents
- What Is Neurotrophic Keratitis?
- Causes of Neurotrophic Keratitis
- Stages of the Disease
- Symptoms (Or Lack Thereof)
- How It Is Diagnosed
- Why Early Detection Is Critical
- Treatment Options
- Living with Neurotrophic Keratitis
- Conclusion
- FAQs
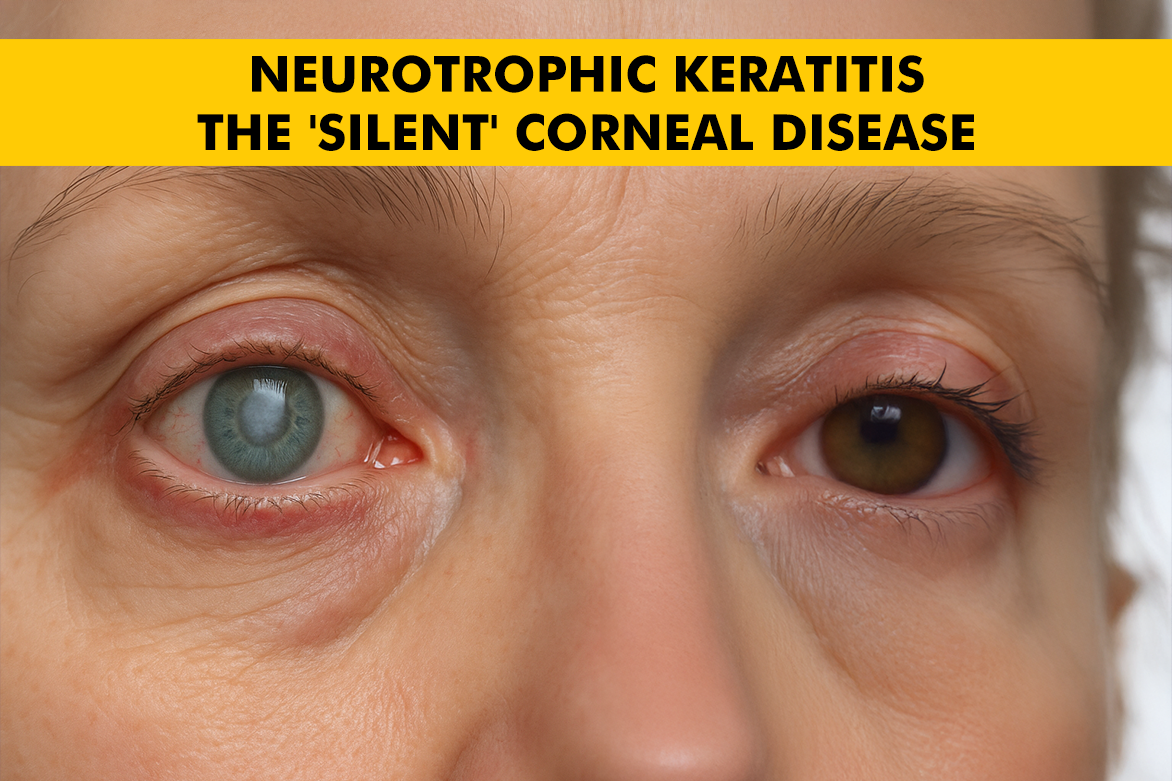
In the space of ocular diseases, some conditions echo in the form of pain and visible symptoms. In case of neurotrophic keratitis (NK), it moves quite silently, causing progressive corneal damage without the well-known warning signs. This silent and rare corneal disorder can lead to irreversible vision loss if left undiagnosed or mismanaged. The absence of pain, despite advanced corneal damage, earns NK its ominous label: the “silent” disease of the eye.
For doctors, general practitioners, and even certain specialists, the absence of pain can be deceptive. Knowledge of this disease, its causes, phases, and treatments, is important to avoid its worst consequences. In this detailed piece, we will explain neurotrophic keratitis, putting light on a disease that usually goes unnoticed.
What Is Neurotrophic Keratitis?
Neurotrophic keratitis (NK) is a rare, degenerative corneal disease. It results from injury to the trigeminal nerve. This nerve supplies sensory innervation to the ocular surface. Upon loss of this sensory input (clinically known as corneal hypoesthesia), the cornea’s capacity to sense injury and activate healing is compromised to a great extent.
The cornea, that is, the transparent cover of the eye, is important for sight. It is filled with sensory nerves that make it one of the most sensitive organs of the body. These nerves are important in keeping the cornea intact. This aids in tear production, blinking, and protecting the immune system. In NK, the breakdown of these nerves leads to a failure of the cornea to properly protect and repair itself.
What makes neurotrophic keratitis particularly dangerous? It is that it usually lacks typical symptoms, especially pain, leading to delayed diagnosis as well as treatment. By the time visual disturbances prompt a consultation, the disease may have already progressed to an advanced stage.
Causes of Neurotrophic Keratitis
Injury to the trigeminal nerve or its branches may happen as a consequence of a host of underlying medical conditions and procedures. Common causes are:
- Herpetic eye infections: This is the most common cause of NK. Both Herpes Simplex Virus (HSV) as well as Herpes Zoster Virus (HZV) can damage the corneal nerves. This can happen either during active infection or because of recurrent inflammation.
- Diabetes mellitus: Unmanaged diabetes is accompanied by peripheral neuropathy. This entails eye nerves that can lower corneal sensitivity.
- Long-term contact lens wear: This happens because of poor hygiene or extended use. The contact lenses can desensitize the cornea and interfere with its protective mechanisms.
- Ocular procedures: LASIK, PRK, and corneal transplant surgery may inadvertently damage corneal innervation.
- Neurological conditions: Diseases such as multiple sclerosis, trigeminal neuralgia, or brainstem strokes can impair nerve function at various levels.
- Chronic inflammatory or chemical injury can also lead to nerve damage and impair ocular surface healing.
Identifying the root cause is important for developing an attuned treatment plan. Also, for preventing recurrence or further progression.
Stages of the Disease
NK is usually classified into three progressive stages, as defined by the Mackie classification:
Stage 1 – Mild (Epithelial changes)
- This is characterized by punctate epithelial erosions.
- These are small, scattered lesions on the corneal surface.
- May be misdiagnosed as dry eye syndrome because of similar superficial appearance.
- Corneal sensitivity is reduced, but the structure is still intact.
Stage 2 – Moderate (Persistent epithelial defect)
- The cornea develops a non-healing epithelial defect that lasts for more than 2 weeks.
- Surrounding epithelial edges may appear rolled or swollen.
- There is now more risk of secondary infection and stromal involvement.
Stage 3 – Severe (Corneal ulceration, melting, or perforation)
- The corneal stroma breaks down. This leads to ulceration, stromal melting, and in severe cases, perforation.
- Risk of permanent vision loss is quite high.
This stage usually needs urgent surgical intervention. Early identification of the disease stage directly influences treatment efficacy and visual prognosis.
Symptoms (Or Lack Thereof)
The most difficult part of diagnosing neurotrophic keratitis is its symptomlessness. Because the trigeminal nerve is affected, the patient does not feel pain despite severe corneal damage.
- Mild redness or ocular discomfort
- Blurry vision secondary to surface irregularity
- Dryness sensation or foreign body sensation
- Impaired wound healing, particularly with trauma or surgery
The most important point is the lack of correlation between severity and symptoms. Even in stage 3, patients can report little pain, and regular eye exams are needed for at-risk patients.
How It Is Diagnosed
Neurotrophic Keratitis diagnosis combines clinical examination with specific testing. The most important diagnostic steps are:
- Slit-lamp examination: To observe corneal epithelial defects, scarring, or ulceration.
- Cochet-Bonnet esthesiometry: A thin nylon filament is used to assess corneal sensitivity. A reduced or absent response is usually a red flag.
- Fluorescein staining: Highlights areas of epithelial damage or defects.
- Clinical history: A comprehensive review of systemic diseases (e.g., diabetes), previous ocular surgeries, infections, or contact lens use.
In the majority of instances, diagnosis is established with a combination of decreased corneal sensitivity and refractory, persistent epithelial defects.
Why Early Detection Is Critical
The absence of pain in NK is deceptive. Unnoticed injuries can worsen rapidly, especially when accompanied by factors like dry eye, infection, retinal detachment, or inflammation. If not addressed early, even a small lesion can evolve into an ulcer or perforation, resulting in:
- Irreversible corneal scarring
- Infection
- Vision loss, sometimes necessitating corneal transplantation
Early detection will stop or reverse the disease process. Regular monitoring, especially in high-risk patients (e.g., diabetic patients or post-LASIK patients), is vital for prevention.
Treatment Options
Management of neurotrophic keratitis is a stage-wise progression and entails stimulating healing, re-establishing corneal integrity, as well as preserving vision.
Stage 1 (Mild)
- Preservative-free artificial tears for lubrication
- Non-usage of contact lenses. Also, potentially toxic eye drops
- Treatment of underlying conditions
Stage 2 (Moderate)
- Autologous serum tears or platelet-rich plasma eye drops to give growth factors
- Bandage contact lenses to shield the epithelium
- Amniotic membrane grafts, used as overlays or sutured grafts
Stage 3 (Severe)
- Cenegermin (Oxervate): It is a groundbreaking therapy. It uses recombinant human nerve growth factor. It has also been shown to notably improve healing by regenerating corneal nerves.
Surgical interventions like:
- Tarsorrhaphy (temporary eyelid closure to protect the cornea)
- Conjunctival flaps
- Corneal transplantation (usually as a last resort)
Each treatment plan is personalized. Also, it depends on disease severity, underlying cause, and response to earlier therapies.
Living with Neurotrophic Keratitis
For individuals diagnosed with NK, lifestyle adaptations and consistent medical follow-up become lifelong priorities. Key management strategies include:
- Regular eye examinations with a corneal specialist
- Protective eyewear to prevent accidental trauma
- Steering clear of topical anesthetics or preserved artificial tears, which can exacerbate the disease
- Regulation of systemic illnesses such as diabetes, which may affect nerve well-being and healing
- Patient education is critical to preventing recurrence and enhancing outcomes.
Neurotrophic keratitis is a rare but blinding condition that requires increased vigilance. Its insidious course, fueled by loss of corneal sensation, tends to cause late presentation. But with modern diagnostics and regenerative treatments such as cenegermin, hope for the preservation of sight, even in severe cases, is real.
Conclusion
Finally, early detection, fine-tuned treatment, and close follow-up remain the pillars of managing this elusive condition. For those at risk or already affected, vigilance as well as specialized care can make all the difference.