Cortical cataract, a common type of age-related cataract, poses a significant impact on vision and quality of life for many individuals. As we age, changes in the lens of the eye can lead to the development of cortical cataracts, affecting the outer layer of the lens known as the cortex. Understanding the causes, symptoms, and available treatments for cortical cataract is crucial for proactive eye care and early intervention. In this blog, we will delve into the intricacies of cortical cataracts, exploring the factors that contribute to their formation, the telltale signs that indicate their presence, and the various treatment options that can restore visual clarity.
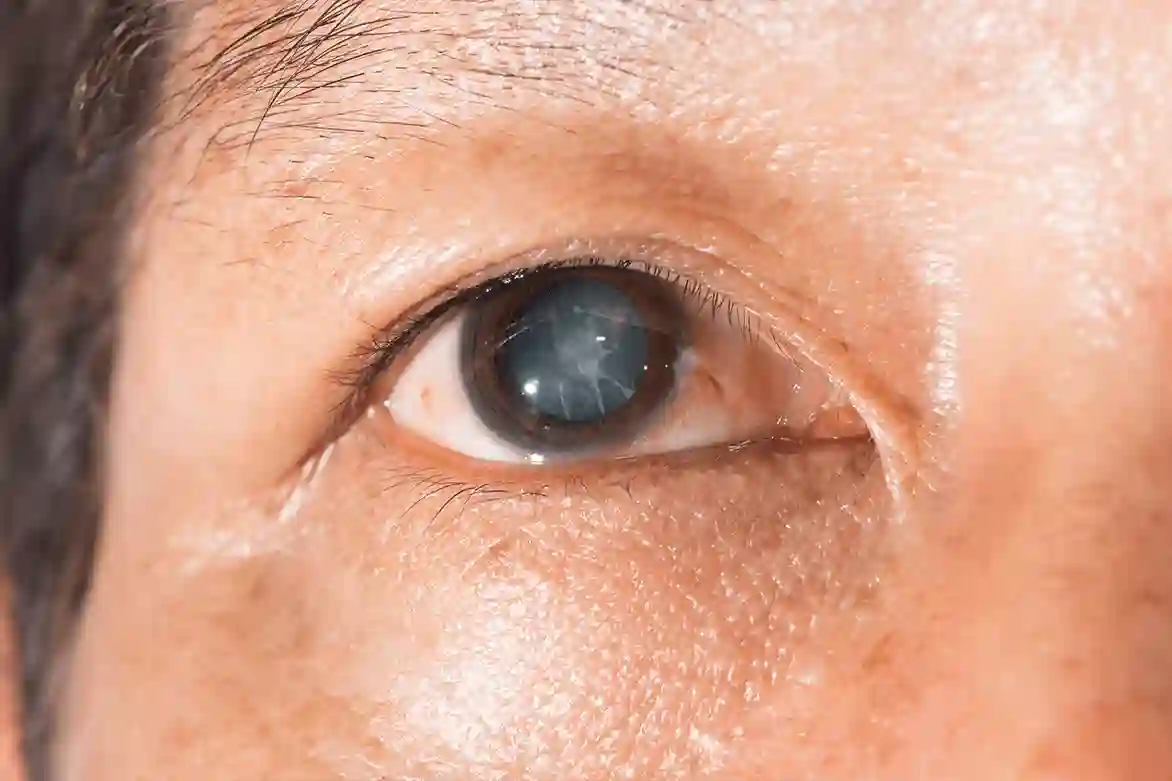
What Is Cortical Cataract?
A cortical cataract is a type of cataract that affects the lens of the eye. It occurs when the outer layer of the lens, called the cortex, becomes opaque and forms wedge-shaped opacities. These opacities can block or scatter light as it enters the eye, causing vision problems.
Cortical cataracts typically develop slowly and progress over time. They are more commonly found in older adults, but can also occur in younger individuals due to certain risk factors such as diabetes, smoking, prolonged exposure to sunlight, and the use of corticosteroid medications.
The exact cause of cortical cataracts is not fully understood, but it is believed to be related to changes in the proteins within the lens. These changes may be due to a combination of genetic factors, aging, and environmental factors.
If left untreated, cortical cataracts can significantly impair vision and affect daily activities. However, with proper diagnosis and treatment, the symptoms can be managed and vision can be improved.
Causes of Cortical Cataract
The exact causes of cortical cataracts are not known, but several factors may contribute to their development. These include:
- Aging: As we age, the proteins in the lens may break down or clump together, leading to the formation of cataracts.
- Genetic Factors: Certain genetic mutations may increase the risk of developing cortical cataracts.
- Diabetes: People with diabetes are more prone to developing cataracts, including cortical cataracts.
- Smoking: Smoking has been linked to an increased risk of cataract formation, including cortical cataracts.
- Prolonged Exposure to Sunlight: Overexposure to ultraviolet (UV) radiation from the sun can accelerate the development of cataracts.
- Corticosteroid Medications: Long-term use of corticosteroid medications, such as prednisone, can increase the risk of developing cataracts.
It’s important to note that while these factors may increase the risk of cortical cataracts, they do not guarantee their development. Some individuals may develop cataracts without any known risk factors.
How Common Are Cortical Cataracts?
Cortical cataracts are a common type of cataract, accounting for about one-third of all cataract cases. They are more prevalent in older adults, particularly those over the age of 60. However, cortical cataracts can also occur in younger individuals, especially if they have certain risk factors such as diabetes or a family history of cataracts. It’s important to have regular eye exams to detect the presence of cortical cataracts and monitor their progression. Early detection can lead to timely treatment and better management of the condition.
Symptoms of Cortical Cataract
Cortical cataracts can cause various symptoms, which may include:
- Blurred or hazy vision
- Difficulty seeing in bright light or glare
- Problems with depth perception
- Changes in color vision
- Double vision in one eye
- Frequent changes in eyeglass prescription
These symptoms can gradually worsen over time and may affect both eyes. If you experience any of these symptoms, it is important to consult an eye care professional for a proper diagnosis and appropriate treatment.
Diagnosis and Treatment Options
Diagnosing cortical cataracts involves a comprehensive eye examination, which may include:
- Visual acuity test: This test measures how well you can see at various distances.
- Slit-lamp examination: A specialized microscope is used to examine the structures of the eye, including the lens.
- Dilated eye exam: Eye drops are used to widen the pupil, allowing the doctor to examine the lens and other parts of the eye.
- Retinal exam: The doctor examines the back of the eye to check for any other eye conditions or complications.
Once diagnosed, the treatment options for cortical cataracts depend on the severity of the symptoms and their impact on daily life. In the early stages, vision can often be improved with prescription eyeglasses or contact lenses. However, as the cataract progresses and vision deteriorates, surgery may be recommended.
Cataract surgery involves removing the cloudy lens and replacing it with an artificial lens called an intraocular lens (IOL). The surgery is typically safe and highly effective in restoring clear vision. It is one of the most commonly performed surgeries worldwide. It’s important to discuss the treatment options with an eye care professional to determine the best course of action based on individual circumstances and preferences for quick post cataract recovery and visual outcomes.
Risks and Complications of Cortical Cataract
While cataract surgery is generally safe, it does carry some risks and potential complications. These may include:
- Infection
- Bleeding
- Swelling
- Retinal detachment
- Glaucoma
- Secondary cataract (posterior capsule opacification)
The risks and complications associated with cataract surgery can vary depending on individual factors, such as overall health and the presence of other eye conditions. It’s important to discuss these risks with an eye care professional before undergoing surgery.
Preventive measures for Cortical Cataract
While it may not be possible to prevent cortical cataracts entirely, certain measures can be taken to reduce the risk and delay their development. These include:
- Protecting the eyes from UV radiation by wearing sunglasses with UV protection
- Quitting smoking or avoiding exposure to secondhand smoke
- Managing chronic health conditions, such as diabetes, through regular medical care
- Eating a healthy diet rich in fruits, vegetables, and antioxidants
- Practicing good eye hygiene and avoiding eye injuries
By adopting these preventive measures, individuals can minimize their risk of developing cortical cataracts and maintain good eye health.
Read about Tips to prevent cataract
Do Cortical Cataracts Require Surgery?
The decision to undergo surgery for cortical cataracts depends on the severity of the symptoms and their impact on daily life. In the early stages, vision can often be managed with prescription eyeglasses or contact lenses. However, as the cataract progresses and vision deteriorates, surgery may be recommended to restore clear vision and improve quality of life.
It’s important to consult with an eye care professional to determine the appropriate treatment plan based on individual circumstances and preferences.
What Happens If You Let Cataracts Go Untreated?
If left untreated, cortical cataracts can significantly impact vision and interfere with daily activities. The symptoms may progressively worsen, making it difficult to perform tasks such as reading, driving, or recognizing faces. Cataracts can also increase the risk of falls and accidents.
It’s important to seek timely treatment for cortical cataracts to prevent further deterioration of vision and improve overall quality of life.
Conclusion:
Grasping the nuances of cortical cataracts empowers individuals to take charge of their eye health and seek timely assistance when needed. Early detection of symptoms and a comprehensive understanding of the available treatments can significantly improve the prognosis for those affected by cortical cataracts. Whether it be lifestyle modifications, prescription eyewear, or surgical interventions, the array of options underscores the importance of tailored approaches to address the unique needs of each patient. As research and technology continue to advance, a proactive approach to eye care ensures that individuals can enjoy a clear and vibrant vision, enhancing their overall well-being as they navigate the golden years.
FAQs
Can cortical cataracts be reversed without surgery?
While there is no known way to reverse the progression of cortical cataracts without surgery, early detection and management of symptoms can help improve vision and slow down the advancement of the cataract.
How long does it take for a cortical cataract to form?
The formation of cortical cataracts is a gradual process that can take months or years. The rate of progression may vary depending on individual factors.
Can you drive with a cortical cataract?
If a cortical cataract significantly affects vision and impairs the ability to see clearly, it may not be safe to drive. It is important to consult with an eye care professional to assess visual acuity and determine if driving restrictions are necessary.
Can diet and lifestyle changes help prevent cortical cataracts?
While a healthy diet and lifestyle can contribute to overall eye health, there is no guarantee that they will prevent the development of cortical cataracts. However, adopting these habits can help reduce the risk and delay the onset of cataracts.
Can cortical cataracts affect both eyes?
Yes, cortical cataracts can affect both eyes, although they may not develop at the same rate or cause identical symptoms in each eye. It’s important to consult with an eye care professional for personalized advice and answers to specific questions regarding cortical cataracts.
Is cortical cataract serious?
Yes, cortical cataracts can be serious as they affect the outer edges of the lens and can lead to vision problems.
What are the stages of cortical cataract?
The stages of cortical cataracts include early, immature, mature, and hypermature.
What are the characteristics of a cortical cataract?
Characteristics of cortical cataracts include white opacities in the lens periphery.
What is the difference between a cortical and a nuclear cataract?
Cortical cataracts affect the outer layer of the lens, while nuclear cataracts impact the center part of the lens.