Table of Contents
- What Is Blue Dot Cataract (Cerulean Cataract)?
- Causes of Blue Dot Cataract
- Early Warning Signs of Blue Dot Cataract
- Complications of Untreated Blue Dot Cataract
- Blue Dot Cataract Treatment Options
- Recovery After Blue Dot Cataract Surgery
- Can Blue Dot Cataracts Be Prevented?
- When Should You Visit an Eye Specialist?
- FAQs
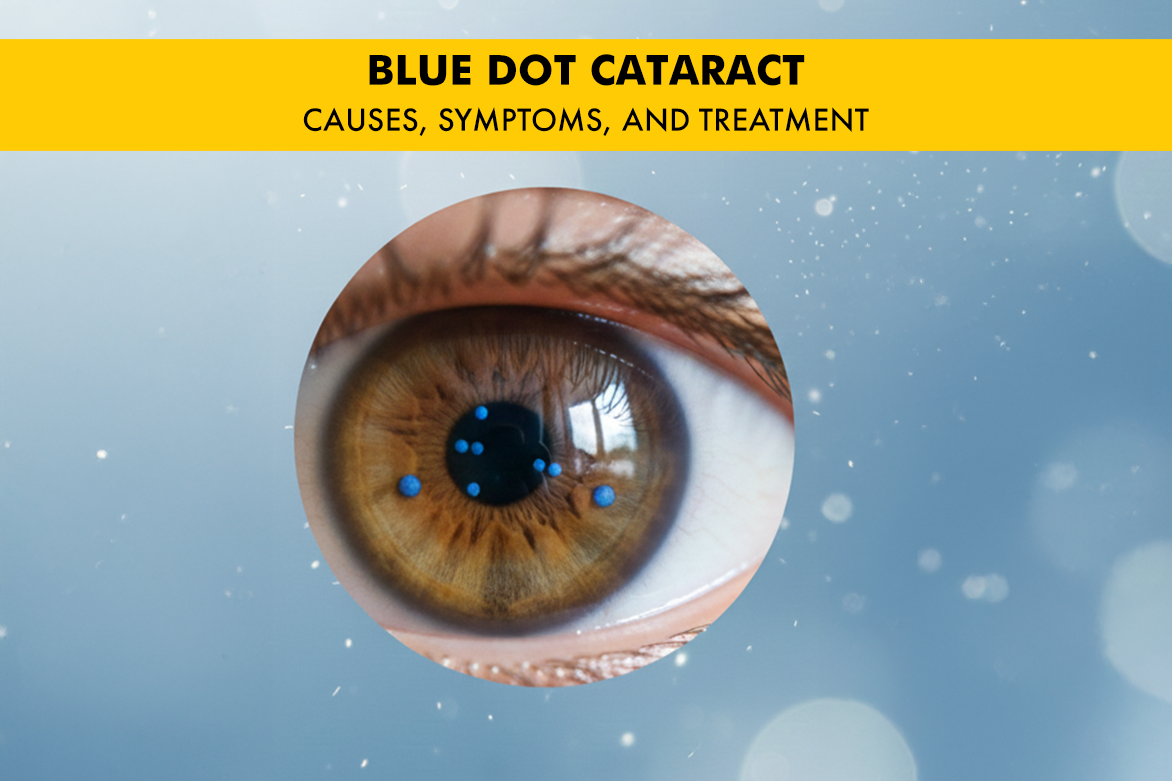
A cataract is a common eye condition where the normally clear lens becomes cloudy. When most people think of cataracts, they think of age-related vision loss. However, the Blue Dot Cataract, or Cerulean Cataract, is slightly different from a natural cataract that we think of. This is a special type of congenital/developmental cataract, meaning it is present at birth or develops during infancy, and is caused by developmental anomalies in the lens.
While usually visually insignificant, understanding this condition is crucial. This article will explore the causes, symptoms, and treatment landscape for this distinct, punctate form of lens opacification.
What Is Blue Dot Cataract (Cerulean Cataract)?
The term ‘Blue Dot Cataract’ perfectly describes its appearance: numerous, tiny, bluish or greyish-white opaque dots scattered within the lens.
How it Differs from Regular Age-Related Cataracts
| Feature | Blue Dot Cataract | Age-Related Cataract |
| Onset | Congenital / Developmental (childhood or young adults) | Acquired (usually after age 40) |
| Opacities | Small, punctate dots scattered mainly in the lens cortex. | Various patterns (nuclear, cortical, subcapsular). |
| Vision Impact | Often mild; significant reduction is less common. | Can lead to severe vision loss if untreated. |
| Progression | Non-progressive or very slowly progressive (stationary). | Progressive, worsening over time. |
| Typical Presentation | Usually Bilateral (in both eyes). | Can be unilateral or bilateral. |
Causes of Blue Dot Cataract
Blue dot cataract cause is primarily genetic and developmental, rooted in errors during the formation of the lens fibres in utero.
- Genetic Inheritance
- Autosomal Dominant Pattern: This is the most common mechanism. The cataract is often passed down through families, making a family history a key risk factor for this inherited eye disorder.
- Gene Mutations: Defects in specific genes that encode lens proteins (crystallins) lead to the formation of abnormal, opaque lens material that crystallises into the distinctive blue dots.
- Association with Systemic Conditions
- Down Syndrome (Trisomy 21): The blue dot cataract in Down syndrome is one of the most frequently observed eye conditions, highlighting the strong link between this developmental cataract and genetic anomalies.
- Who Is at Risk?
- Individuals with a strong family history of congenital/developmental cataracts.
- Children diagnosed with Down Syndrome.
- Children exposed to certain maternal infections (like Rubella) during development, although the blue dot form is less commonly associated than other types of congenital cataract.
Early Warning Signs of Blue Dot Cataract
Warning Signs in Adults
- Slightly Blurred or Dim Vision (SV): The most common reported symptom, usually mild.
- Reduced Contrast Sensitivity: Difficulty seeing fine details or distinguishing objects in dim light.
- Glare and Halos: Increased light scatter, leading to increased sensitivity to bright light, glare, or halos around headlights at night.
- Colours: May appear slightly less vivid or saturated.
Warning Signs in Children
- The child is sitting too close to screens or holding toys very near their face.
- Squinting or persistent head tilting.
- Struggling in low light or overcast conditions.
Complications of Untreated Blue Dot Cataracts
Since the blue dot cataract is typically mild and non-progressive, the risk of severe complications is low in adults. However, in infants and young children, even mild visual obstruction can be serious: If a cataract is visually significant, the brain may ignore the blurry input, leading the visual pathway to fail to develop properly. This results in permanent vision loss if not corrected promptly.
Blue Dot Cataract Treatment Options
Treatment is tailored to the severity of the vision impairment.
Observation (The Most Common Approach)
If the vision is good and the opacities are peripheral, no immediate intervention is required. Patients are placed on observation with annual eye check-ups to monitor for any changes.
Blue Dot Cataract Surgery (Cataract Extraction)
Surgery is recommended when the patient’s vision falls below the functional threshold for their daily life, or if the cataract poses a threat of amblyopia in a child.
| Patient Group | Indication for Surgery | Procedure |
| Adults | Significant impact on vision (e.g., difficulty driving or reading). | Surgery: The cloudy lens is removed using ultrasound, and a clear, artificial intraocular lens (IOL) is implanted. |
| Children | The cataract is dense enough to risk amblyopia. | Timely cataract removal (often without IOL in very young infants) followed by aggressive visual rehabilitation. |
Recovery After Blue Dot Cataract Surgery
Recovery is generally smooth, but strict adherence to post-operative instructions is vital.
- Post-surgery Care: Use prescribed antibiotic and anti-inflammatory eye drops religiously. Wear a protective eye shield, especially at night, for the first few days.
- Visual Improvement Timeline: Initial improvement is often seen within days. Maximum visual recovery typically occurs over 4–6 weeks.
- Follow-up Visits: Regular check-ups are essential to monitor healing, check the IOL position, and ensure the best visual outcome. For children, follow-up vision therapy (like patching) is critical.
Can Blue Dot Cataracts Be Prevented?
Since this is a congenital condition primarily linked to genetics, Blue Dot Cataracts cannot be prevented. However, the focus should be on early detection and proactive management to prevent permanent vision deficits, especially amblyopia, in children.
When Should You Visit an Eye Specialist?
If you have a known family history of congenital eye conditions, or if you or your child exhibits any of the symptoms like glare, blurry vision, or difficulty seeing in low light, schedule an appointment with an eye specialist immediately. Early intervention is key to preserving sight.