Key Takeaways:
|
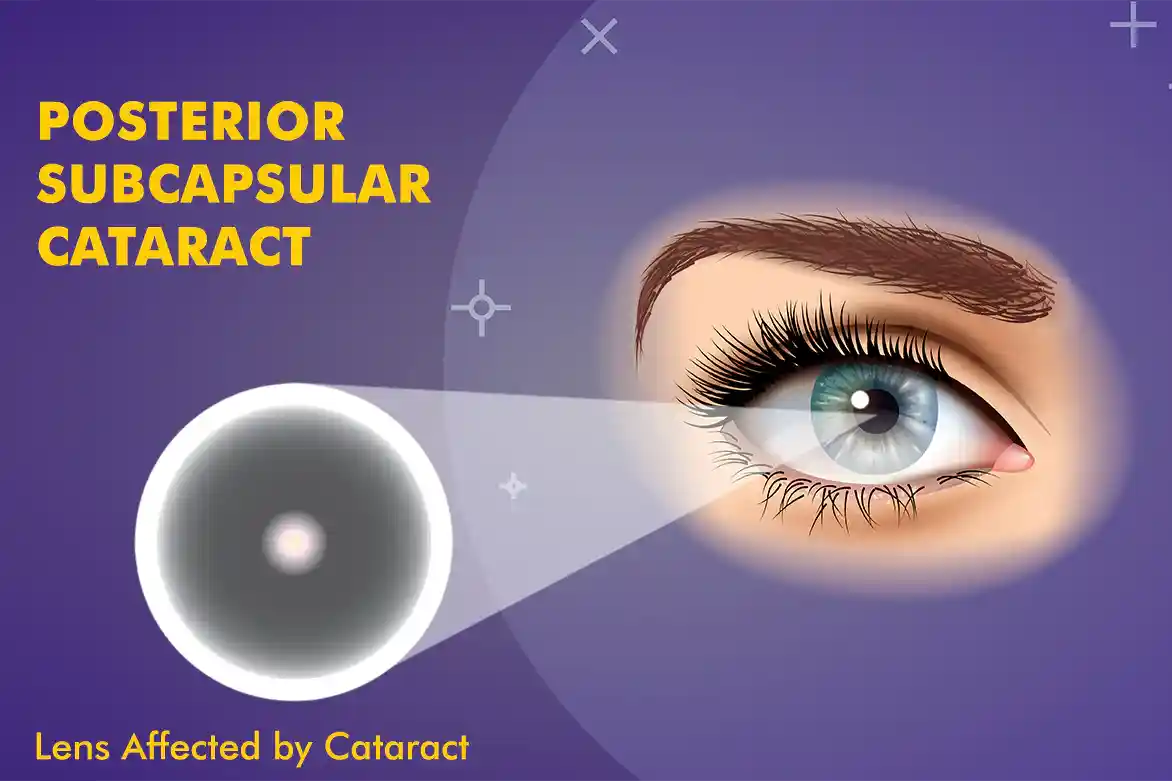
A posterior subcapsular cataract (PSC) is a type of cataract that forms at the back of the eye’s natural lens, just in front of the posterior capsule that encases the lens. Unlike other cataract types, which may affect the centre (nuclear) or edges (cortical) of the lens, PSC specifically targets the back layer. This location is critical because it lies directly in the path of light entering the eye, which can significantly interfere with vision, particularly in bright environments or while reading.
In medical practice, PSC is often more visually disabling than other types of cataracts, even when smaller in size. Individuals frequently report a sudden onset of symptoms rather than a slow progression, making it an important diagnosis in clinical ophthalmology.
In this guide, you’ll find what PSC cataract symptoms look like, the main causes and risk factors, how doctors grade PSC, and the treatment/surgery options.
What is Posterior Subcapsular Cataract (PSC)?
A posterior subcapsular cataract (PSC) is a cloudy patch that forms at the back of the eye’s lens, right in front of the thin “capsule” that holds the lens in place. Because this spot sits directly in the path of light, it can blur vision even when the cataract is small.
PSC feels different from other cataracts. While nuclear cataracts affect the centre of the lens and cortical cataracts start at the edges, PSC sits at the back layer, so bright light, headlights, and reading up close become difficult. Many people notice glare and halos and report that their vision worsens faster than they expected.
Doctors pay close attention to PSC because its position can reduce vision more quickly than other types. The good news is that it is treatable, and your eye specialist can guide you on the timing and the best treatment plan.
Anatomy of the Lens
To explain the anatomy of a lens, think of the eye’s lens as a clear, flexible disc that sits just behind the iris (the coloured black part). Its job is to focus light onto the retina so you see a sharp picture. The lens is wrapped in a thin, transparent bag called the capsule; the front of this bag is the anterior capsule, and the back is the posterior capsule.
A posterior subcapsular cataract (PSC) forms right under the back (posterior) capsule. Tiny lens cells in this area can change in an abnormal way and create small, cloudy spots. Because these sit exactly where light passes through, even a small PSC can block light and cause glare, halos, and blur, especially in bright light or while reading.
How a PSC Develops
Posterior subcapsular cataracts develop when some lens cells drift toward the back of the lens and start to clump together. These clumps turn into grainy or plaque-like opacities, the early footprint of a PSC.
Different things can trigger this, such as long-term steroid use, diabetes, eye injury, radiation exposure, or other health issues. Unlike a nuclear cataract, which takes years to grow, PSC can progress faster. Many people notice that their near vision and bright-light vision get worse sooner than expected.
PSC can also appear in both eyes, especially when linked to systemic causes like steroids or diabetes. The good part is that once it’s confirmed, your eye doctor can track its pace and plan timely treatment, so you can keep doing the things you love.
Common Causes of PSC
Common causes for posterior subcapsular cataract (PSC) are long-term steroid use, diabetes, eye injury, radiation exposure, or other health issues.
When we identify the cause, we can monitor it more closely and sometimes reduce the risk.
| Cause | How it can lead to PSC? |
| Long-term steroids | Steroids change lens cells at the back of the lens, creating cloudy spots. |
| Diabetes | High blood sugar upsets lens chemistry and speeds clouding at the back. |
| Eye injury (trauma) | A hit or cut to the eye damages lens fibres and triggers back-of-lens haze. |
| Radiation / strong UV | Radiation and years of strong sun can alter lens cells and form PSC. |
- Prolonged corticosteroid use
Steroids are powerful medicines, but long-term use, such as tablets, inhalers for asthma, skin/eye drops, or injections, can speed up PSC.
Prevention: If you need to use steroids for a long time, your doctor should suggest regular eye checks to catch changes early.
- Diabetes mellitus
When blood sugar stays high, the lens chemistry shifts. Over time, this can cloud the back of the lens and form a PSC.
Prevention: Good sugar control and routine eye exams help spot problems sooner.
- Ocular trauma (eye injury)
A blunt hit or penetrating injury can disturb the lens fibers. After an injury, a PSC may appear quickly or months later.
Prevention: Wearing protective eyewear for work and sports is a simple way to lower the risk.
- Radiation exposure
Radiation therapy near the eyes (for head/neck cancers) and years of strong UV light can change lens cells and trigger PSC.
Prevention: Using UV-blocking sunglasses and a hat outdoors is a smart habit.
Posterior Subcapsular Cataract Risk Factors
Below are the risk posterior subcapsular cataract risk factors:
| Risk factor | Why it raises risk/notes |
| Age (40+) | Natural lens changes make clouding at the back more likely. |
| Chronic steroid use (inhaled, oral, skin/eye drops) | Long-term steroids can alter lens cells and speed PSC. |
| Systemic diseases (e.g., lupus, sarcoidosis) | Inflammation and medicines used can affect the lens. |
| Family history of cataracts | Genes can make the lens more prone to clouding. |
| Past eye surgery or uveitis | Inflammation or surgical changes can trigger back-of-lens haze. |
| Radiation / strong UV exposure | Radiation and years of sun can damage lens cells. |
Symptoms for Posterior Subcapsular Cataract (PSC)
A posterior subcapsular cataract (PSC) bothers you more than its size because it sits right in the light’s path. Many people first notice trouble in bright light or when doing near work. These problems are more noticeable during reading, computer use, and night driving.
- Blurry or hazy vision, especially in sunlight or with bright indoor lights
- Reading becomes hard, small print fades or swims
- Glare and halos around headlights and streetlights at night
- Lower contrast greys look washed out, and colours seem dull
- Faster change in vision than expected, sometimes more in one eye
- Light sensitivity, needing shades or dimmer screens
Diagnosis for Posterior Subcapsular Cataract (PSC)
Diagnosing a posterior subcapsular cataract involves a full eye exam to confirm PSC and rule out other issues. The process includes:
Step 1: Visual Acuity Test
Reading the eye chart shows how clearly you see.
Step 2: Slit-lamp Exam
With a microscope and a thin beam of light, the doctor looks at the lens. A PSC appears as a grainy or plaque-like patch at the back of the lens.
Step 3: Dilated Fundus Exam
Although PSC affects the lens, not the retina, dilation helps widen the pupil, allowing the doctor to examine the retina and optic nerve for any other problems that might affect vision. If the PSC is early and mild, your doctor watches and rechecks at intervals. If it’s advanced or clearly affecting daily life, they’ll discuss treatment options, usually cataract surgery with an artificial lens to restore clearer vision.
Posterior Subcapsular Cataract (PSC) Progression
A posterior subcapsular cataract (PSC) progression can move at different speeds.
In some individuals, it remains stable for months, while in others, it progresses quickly. Because PSC sits right in the visual axis, even a small change can feel big in daily life. You notice growing trouble with night driving, reading, or working under bright/fluorescent lights. When these tasks start to limit your routine, it’s a sign to discuss posterior subcapsular cataract surgery with your eye doctor.
Posterior Subcapsular Cataract (PSC) Treatment Options
Posterior subcapsular cataract (PSC) treatment starts by meeting an eye specialist. The plan depends on how bad the symptoms are and how much your vision is affected. Simple steps can help for a while, but the definitive treatment is usually surgery.
Non-Surgical Approaches (short-term help)
- Stronger glasses for the early stages.
- Anti-glare lenses or sunglasses to reduce light sensitivity.
- Lifestyle changes like limiting night driving and using bigger fonts on screens.
These measures can make life easier, but they do not stop PSC from progressing.
Surgical Approach (long-term solution)
When non-surgical steps aren’t enough, cataract extraction is the standard care. Surgery is outpatient with local anaesthesia. Many people notice clearer vision within a few days.
Phacoemulsification: The surgeon makes a small incision, uses ultrasound to break the cloudy lens into tiny pieces, removes them, and places a clear intraocular lens (IOL) in the natural lens capsule.
Laser-assisted option (FLACS): In some centres, a femtosecond laser helps with precise cuts and lens pre-softening. Your surgeon will advise if this adds value for your eye.
Posterior Subcapsular Cataract (PSC) Recovery
Good aftercare helps you heal smoothly and protects your result.
- Use the prescribed eye drops ( antibiotic and anti-inflammatory) exactly as directed.
- Avoid rubbing the eye, heavy lifting, and bending low in the first days.
- Wear a protective shield at night and sunglasses outdoors.
- Keep your follow-up visits so the doctor can track healing and update any glasses.
| Important:
Most patients are back to routine activities within a week, while full visual stabilisation can take a few weeks. If anything feels wrong, pain, a sudden drop in vision, or increasing redness, contact your eye doctor right away. |
Conclusion
A posterior subcapsular cataract (PSC) sits at the back of the lens, right in the light’s path, so even a small patch can cause big problems with glare, bright light, and near work. Simple measures (stronger glasses, anti-glare lenses) can help for a while, but when daily life is affected, posterior subcapsular cataract surgery is the reliable fix. With the right timing and lens choice, most people regain clear, comfortable vision.
FAQs
What are the main causes of posterior subcapsular cataract?
The main causes for posterior subcapsular cataract are long-term steroid use, diabetes, eye injury, and radiation/strong UV exposure; age and inflammation can also play a role.
What are the common symptoms to watch for in Posterior Subcapsular Cataract?
The common symptoms to watch for posterior subcapsular cataract are glare and halos in bright light or at night, blur for near tasks like reading, light sensitivity, and reduced contrast.
How is Posterior Subcapsular Cataract diagnosed?
Posterior subcapsular cataract is diagnosed with a comprehensive eye exam, such as vision chart testing, a slit-lamp view showing a grainy/plaque-like patch at the back of the lens, and a dilated exam to check overall eye health.
What treatment options are available for Posterior Subcapsular Cataract?
The treatment options for posterior subcapsular cataract include short-term aids (such as stronger spectacles, anti-glare lenses, and lighting adjustments) and definitive surgery to remove the cloudy lens and replace it with a clear IOL when symptoms significantly limit daily life.
What is the recovery process like after cataract surgery for posterior polar cataracts?
The recovery process after cataract surgery for posterior polar cataracts is day-care, but surgeons take extra care because the back capsule can be fragile; you’ll use drops for a few weeks and avoid heavy activity briefly.
Are there any complications associated with cataract surgery for posterior polar cataracts?
The complications associated with cataract surgery for posterior polar cataracts include a higher risk of capsule tear during surgery, plus the small risks (infection, swelling, pressure changes), which your surgeon plans to minimize.
Can posterior polar cataracts recur after cataract surgery?
No, posterior polar cataracts cannot recur after surgery because the cloudy lens is removed. Later, a treatable condition known as posterior capsule opacification (PCO) may appear and can be cleared with a quick YAG laser if needed.
Can a posterior subcapsular cataract be fixed?
Yes, a posterior subcapsular cataract can be fixed with cataract surgery, which removes the cloudy lens and replaces it with a clear IOL; non-surgical steps only ease symptoms temporarily.
How fast do posterior subcapsular cataracts grow?
Posterior subcapsular cataracts grow faster than other types, sometimes months to a few years, so regular check-ups help decide the right time for surgery.
Where is the posterior subcapsular area?
The posterior subcapsular area is just in front of the back (posterior) capsule of the lens, the last layer the light crosses before reaching the retina.
What causes a posterior subcapsular cataract to form compared to other cataract types?
Posterior subcapsular cataract form, compared to other types, is cell changes at the back of the lens, while nuclear or cortical types start in the center or edges of the lens.
What are the early signs of posterior subcapsular cataract?
The early signs of posterior subcapsular cataract are glare in bright light, trouble reading small print, and halos at night, even when distance vision still seems fair.
Is surgery always required for posterior subcapsular cataracts?
No, surgery is not always required for posterior subcapsular cataracts. If symptoms are mild, doctors may monitor and adjust glasses, but surgery is advised when vision limits daily tasks.
How successful is posterior subcapsular cataract surgery?
Posterior subcapsular cataract surgery is highly successful for most people, with clearer vision typically achieved within days to weeks; final results depend on the overall eye health and the chosen lens.