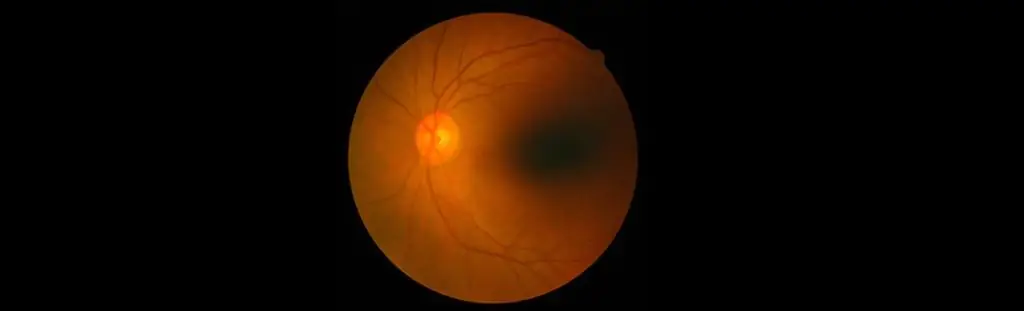
Imagine it’s just a regular day and you are doing your daily chores, suddenly, you see a flash of light and maybe some floaters. You may feel a little nauseous instantly and then there are chances that you do nothing about it. Much later, you may feel a blurry vision. One may panic at this point. A good eye consultation is required without any delay. Such symptoms could be of retinal detachment. Read this piece of information to understand more. It is a detachment or tearing of the retina from its supporting tissues that provide the retina with oxygen nourishment and further connects the received image to the brain. It implies an emergency where one has to immediately rush to the hospital as the chances of partial or total vision loss is expected. Sudden flashes of light, spots, or multiple floaters are the most basic symptoms of retinal detachment. One may start having blurry visions or feel a curtain-like shadow over the visual field; even the peripheral vision starts diminishing. Please note that the aforementioned primary symptoms are painless. You may not experience any pain and may get away from the situation, thinking it’s nothing important, but if left unattended, partial or complete vision loss is the final destination. It’s also important to note the type of retinal detachment that one may experience; there are three types-
- Rhegmatogenous Retinal Detachment-
Being the most common type of retinal detachment, it occurs through a hole in the retina. It results in the flow of fluid from within the eye to get behind the back of the retina. This interrupts the supply of oxygen and essential nutrients that are received by the retina.
- Tractional Retinal Detachment-
Familiar among people with a poorly managed diabetes-this type of detachment occurs when the scar tissue of the retina contracts and pulls away from the cells and tissues that are connected with the retina.
- Exudative Retinal Detachment-
Abnormal development, lack of protein, cancer behind the retina, inflammation, or any fluid accumulation in the back of the eye results in Exudative Retinal Detachment.
Other reasons for retinal detachment are nearsightedness and at times even after LASIK surgery, cataract surgery, tumors, or other eye diseases may cause the retina to pull away. The risk of retinal detachment also increases among people who have a history of retinal detachment running in their family, or they are over 50 years of age, etc. But since retinal detachment can occur anytime and in anyone, with or without any prior warning or history, what happens once you have rushed to the hospital and waiting for treatment to bring back your complete vision? The sooner the retina is attached back, the better it is. Retinal specialists are the ones who engage in this type of surgery. Depending on the type and cause, the following retinal detachment treatments are provided-
- Scleral Buckling Surgery –
Being the most common type of surgery in case of retinal detachment, the procedure consists of putting up a small piece of a band made of plastic or silicon on the sclera of the eye. The band helps in compressing the eye inwardly and allowing the retina to attach internally.
- Vitrectomy –
In this type of surgery, the posterior chamber of the eye that is the clear jelly-like substance is removed from the eye and is replaced with a clear silicon oil that helps in pushing back the detached retina into its place.
- Pneumatic Retinopexy –
In this method, a small bubble of gas is introduced in the vitreous body of the eye that works to push the detached retina back in its space.
Other treatments also include fixing the retina back through the laser method, which is also called cryopexy. However, surgical reattachments depend a lot on factors like location, cause, the extent of detachment, etc. that impact the success of the surgery. The recovery post-treatment may take 3 to 6 weeks. Depending on the nature of your treatment, the doctor would provide you with a list of instructions to be followed during the recovery period. However, there is no known way of preventing retinal detachment from occurring, but if you are struggling with the thought of being prone to retinal detachment, then here are some quick ideas that you can adapt to skip the risk of the condition that is retinal detachment-
- Wear protective glasses when playing sports or other activities to avoid any injury
- Make a constant effort to control the diabetes level
- If you are highly nearsighted, regular check-ups with the doctor are important
- If retinal detachment has a history running in the family, immediately get a thorough and in-depth dilated eye exam
It is essential to be cautious and proactive when it’s about your vision. Keeping track of your eye’s health must be a part of your routine, whether you are or not prone to the possibility of retinal detachment. When you associate with Centre For Sight , you are given a holistic approach for any kind of eye problem. Do not delay in case you are facing any eye issue even if minute.